
5 Signs of a Bad Tummy Tuck Gone Wrong
A tummy tuck, also known as abdominoplasty, is a cosmetic surgery performed on the abdomen region. The goal is to achieve an improved look at

A tummy tuck, also known as abdominoplasty, is a cosmetic surgery performed on the abdomen region. The goal is to achieve an improved look at

Sydney [Australia]: While dropping weight can be a thankless process, a new study by the University of South Australia indicates that a handful of almonds

Adelaide [Australia]: Millions of people worldwide believe that fitness trackers, pedometers, and smart watches motivate them to exercise more and lose weight, according to a
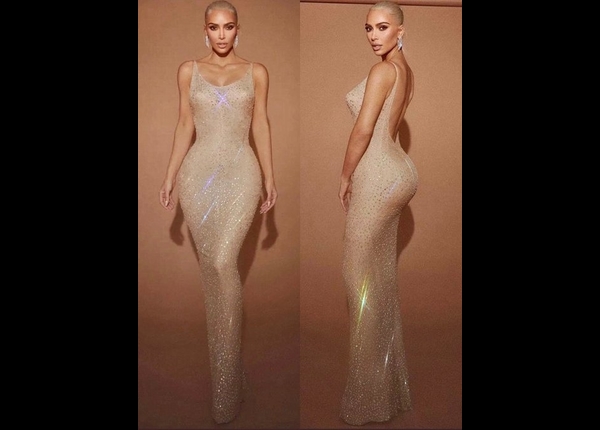
Washington [US]: American TV personality Kim Kardashian, who stepped out for the 2022 Met Gala as a Marilyn Monroe look-alike, has revealed the lengths she

Ajith has joined forces with director H Vinoth for the third continuous time, and the film tentatively titled ‘AK 61’ kickstarted with a puja in April. Ajith celebrated

Washington [US], March 19 (ANI): There are no fertility benefits from weight loss, a recent clinical study has confirmed. The findings of the study were

Washington [US], March 14 (ANI): A new study has found that there are no fertility benefits from weight loss. The findings of the study were

Oxford [England], February 13 (ANI): A new study has shed light on the connection between weight loss and the risk of cancer. The study in

Washington [US], January 19 (ANI): A new study has found that women with obesity and unexplained infertility who lost weight prior to starting infertility treatments

According to new research by Chalmers University of Technology, eating whole grain rye products instead of refined wheat alternatives can offer worthwhile health benefits. The

A study has found that focusing less on structured exercise, and more on building frequent periods of enjoyable movements into the day, will more likely

A new study has found that video-based exercise and weight loss programs with online educational support improved pain and function in people with knee osteoarthritis

Scientists have identified a method of safely mimicking weight-loss benefits of a plant compound that holds critical answers to developing therapies for obesity. The findings

According to a new study review led by University of Illinois Chicago researchers, intermittent fasting can produce clinically significant weight loss as well as improve

A new study has found that weight loss of 15 per cent or more should become a central focus of managing type 2 diabetes (T2D)

The reproductive function in obese boys can be improved through weight loss, which in turn could protect their fertility in adulthood, according to new research.

Choreographer-director Remo D’Souza is proud of his wife and producer Lizelle D’Souza for her grit and determination to undergo an inspiring weight loss transformation. Taking

A tummy tuck, also known as abdominoplasty, is a cosmetic surgery performed on the abdomen region. The goal is to achieve an improved look at

Sydney [Australia]: While dropping weight can be a thankless process, a new study by the University of South Australia indicates that a handful of almonds

Adelaide [Australia]: Millions of people worldwide believe that fitness trackers, pedometers, and smart watches motivate them to exercise more and lose weight, according to a
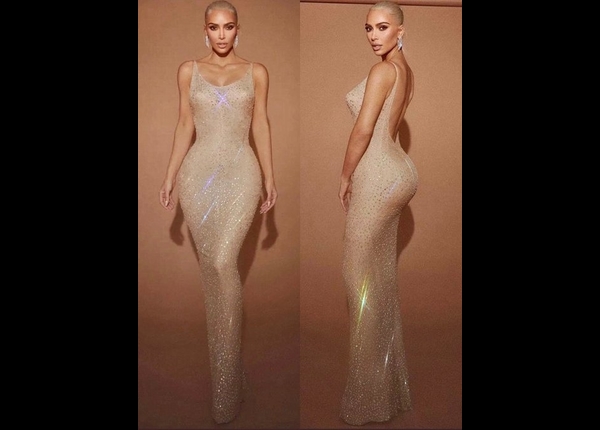
Washington [US]: American TV personality Kim Kardashian, who stepped out for the 2022 Met Gala as a Marilyn Monroe look-alike, has revealed the lengths she

Ajith has joined forces with director H Vinoth for the third continuous time, and the film tentatively titled ‘AK 61’ kickstarted with a puja in April. Ajith celebrated

Washington [US], March 19 (ANI): There are no fertility benefits from weight loss, a recent clinical study has confirmed. The findings of the study were

Washington [US], March 14 (ANI): A new study has found that there are no fertility benefits from weight loss. The findings of the study were

Oxford [England], February 13 (ANI): A new study has shed light on the connection between weight loss and the risk of cancer. The study in

Washington [US], January 19 (ANI): A new study has found that women with obesity and unexplained infertility who lost weight prior to starting infertility treatments

According to new research by Chalmers University of Technology, eating whole grain rye products instead of refined wheat alternatives can offer worthwhile health benefits. The

A study has found that focusing less on structured exercise, and more on building frequent periods of enjoyable movements into the day, will more likely

A new study has found that video-based exercise and weight loss programs with online educational support improved pain and function in people with knee osteoarthritis

Scientists have identified a method of safely mimicking weight-loss benefits of a plant compound that holds critical answers to developing therapies for obesity. The findings

According to a new study review led by University of Illinois Chicago researchers, intermittent fasting can produce clinically significant weight loss as well as improve

A new study has found that weight loss of 15 per cent or more should become a central focus of managing type 2 diabetes (T2D)

The reproductive function in obese boys can be improved through weight loss, which in turn could protect their fertility in adulthood, according to new research.

Choreographer-director Remo D’Souza is proud of his wife and producer Lizelle D’Souza for her grit and determination to undergo an inspiring weight loss transformation. Taking